Clinical services for patients of dementia at NIMHANS
A step towards Dementia Care
Dementia is a growing health crisis in India and the globe, affecting millions of elderly individuals. At the Cognitive Disorders Clinic at the National Institute of Mental Health and Neurosciences (NIMHANS), Bangalore - we aim to look at a multidisciplinary approach to dementia care.
What is Dementia
Dementia is an umbrella term to describe symptoms affecting memory and other cognitive functions such as decision making, language, orientation, and more. People affected with dementia are unable to perform daily activities independently. There are various causes of dementia which causes brain atrophy and degeneration of nerve cells, thus affecting the overall cognitive abilities of the individual.
These symptoms are beyond ‘normal’ or ‘healthy’ aging; often affecting mental, personal, physical and social well-being.
In India, around 1 in every 13 to 14 people aged 60 and above is affected by dementia. The Lancet Commission forecasted a global prevalence of dementia in 2050 at 152.8 million, which is a huge leap from the current numbers of 57.4 million cases. The Lancet has also provided a list of 14 risk factors which are modifiable to delay the onset of dementia.
There is a need to address the Global Burden of Dementia by advancing research, providing multidisciplinary care and increasing awareness on Dementia.
Causes of Dementia
Dementia can be caused by various genetic and lifestyle factors which affect brain health. There are some reversible causes of dementia such as:1. Drug Toxicity: caused by excessive consumption or exposure to alcohol, heavy metals, carbon monoxide
2. Metabolic Causes: such as hepatic/ renal insufficiency, Wilson’s disease
3. Trauma: such as chronic subdural hematoma
4. Neurological causes: such as multiple sclerosis, tumor, normal pressure hydrocephalus
5. Infections: such as chronic meningitis, fungal infections, Tuberculosis, HIV, Creutzfeldt-Jakob disease
6. Collagen vascular disease: such as sarcoidosis or Systemic lupus erythematosus (SLE)
7. Endocrine disorders: such as thyroid or parathyroid
8. Nutritional Deficiency: such as Vitamin B12, Thiamine deficiencies, etc.
Along with this, research continues to explore environmental causes to dementia, which are explored and listed as Risk Factors below.
Risk factors of Dementia
The Lancet commission has identified 14 potential risk factors for dementia which, when controlled, can delay and manage the symptoms of dementia. They are: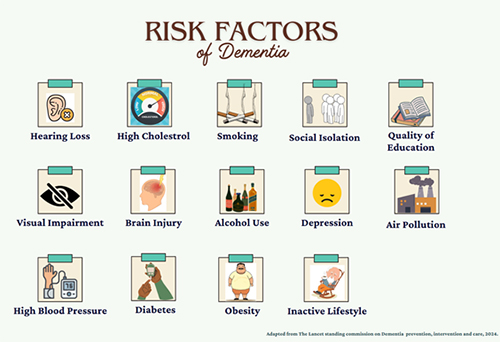
1. Hearing Loss
2. Visual Impairment
3. High Cholesterol
4. High Blood pressure
5. Brain Injury
6. Diabetes
7. Chronic smoking
8. Alcohol Use
9. Obesity
10. Social Isolation
11. Depression
12. Social Withdrawal
13. Quality of Education
14. Air Pollution
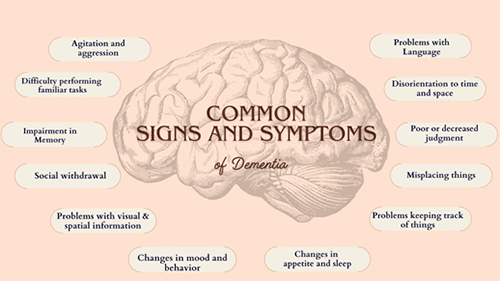
Common Symptoms
Dementia occurs as a combination of symptoms which can vary in intensity and onset. Some common symptoms include:
1. Memory loss: Difficulty in recalling recent events, names of familiar members,
2. Disorientation: Unable or confused about the time, date, place and even self
3. Poor or decreased judgement: Unable to make decisions that were done with ease previously
4. Visuo-spatial Problems: way finding difficulty, unable to find familiar places
5. Changes in mood and behaviour: easily agitated, aggressive, emotional and anxious
6. Changes in sleep and appetite: increase/ decrease in appetite and sleep, sudden changes in preference for food, night terrors, etc.
7. Social withdrawal: Lack of interest or no involvement in social gatherings
8. Problems with Language: difficulty in speaking, understanding or following instructions
9. Delusions: Beliefs about someone trying to harm them/ steal their money/ suspicion
10. Hallucinations: Seeing, hearing, feeling, things that are not actually there.
Subtypes of Dementia
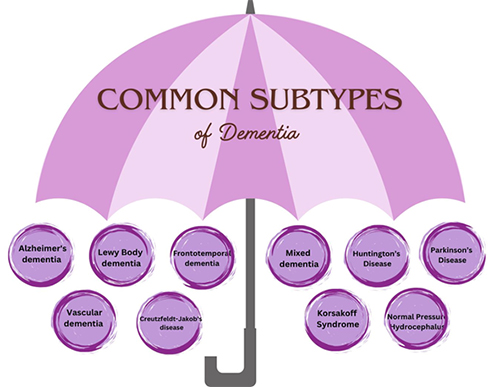
Dementia can be classified into various subtypes depending on the cause, symptoms and changes in brain physiology. The most common subtypes of dementia are:
1. Alzheimer's Disease:
Alzheimer’s disease (AD) is the most common type of dementia which is characterised by changes in memory and other cognitive functions. It typically affects individuals above the age of 60.
Causes: Abnormal deposits of proteins from amyloid plaques and tau tangles in the brain
Symptoms: Memory impairment, wandering/ getting lost, difficulty recognising familiar people, impulsive behaviour, changes in language
2. Vascular Dementia Vascular dementia is a general term to describe changes in cognitive functioning like problem solving, reasoning, planning, etc., caused by impaired blood flow to the brain
Causes: Disrupted blood flow and/or blood clots in the brain
Symptoms: Inability to recall past events, misplacing items, difficulty in making decisions and following instructions, delusions/hallucinations
3. Dementia with lewy bodies
This type of dementia is characterised by specific protein deposits, generally termed as ‘lewy bodies’ which affect the brain’s chemistry
Causes: Abnormal deposits of alpha-synuclein protein or ‘lewy bodies’
Symptoms: Inability to pay attention, disorganised in ideas and speech, rigidity of muscles, loss of coordination, reduced facial expression, problems with sleep such as insomnia or daytime sleepiness
4. Frontotemporal dementia
In frontotemporal dementia, the symptoms caused are due to the changes in the frontal and temporal parts of the brain.
Causes: Atrophy or shrinkage in frontal/temporal parts of the brain, abnormal amounts of tau proteins or TDP-43 proteins inside neurons of the frontotemporal regions of the brain
Symptoms: Difficulty planning,organizing, etc., impulsive behaviors, difficulty managing emotions, movement related issues such as tremors, imbalance, language problems such as difficulty in understanding or speaking.
Other types also include:
5. Mixed dementia: a type of dementia that has symptoms and causes of one or more dementia
6. Creutzfeldt-Jakob’s Disease: a rare type of dementia which is caused by an infectious protein in the brain cells called a ‘prion’. Symptoms include personality changes, memory loss, sudden jerky movements, problems with vision, problems with swallowing, hallucinations, etc.
7. Korsakoff Syndrome: Caused by a severe thiamine deficiency and increased alcohol intake, Korsakoff’s is characterised by changes in learning new information, memory difficulties, confabulation or making new information and even hallucinations.
8. Huntington’s Disease: It is a progressive brain disorder caused by a defective gene which causes changes in the central regions of the brain. Symptoms include uncontrolled movement in limbs, changes in memory and higher order functions such as decision making, etc., mood related concerns such as anxiety, depression and in some cases, even obsessive-compulsive tendencies.
9. Parkinson’s Disease Dementia: This condition develops among some individuals a year into developing Parkinson’s Disease. Symptoms include changes in reasoning skills, problems with language and speech, hallucinations, delusions, changes in mood and disturbances in sleep.
10. Normal Pressure Hydrocephalus: Caused by the accumulation of excess cerebrospinal fluid in the brain’s ventricles, this condition causes symptoms such as changes in movement/gait, changes in memory, reasoning abilities, changes in personality as well as loss of bladder control.
Treatment Options
The number of people living with dementia is rising in India and there is a compelling need to support families through early diagnosis, comprehensive treatment, and preventive strategies.Dementia treatment is mainly symptom management, slowing down disease progression, and enhancing quality of life through pharmacological and non-pharmacological interventions.
1. Pharmacological Treatments
● Cholinesterase Inhibitors (e.g., donepezil, rivastigmine, galantamine) improve cholinergic neurotransmission and are mainly used in Alzheimer's disease.
● NMDA Receptor Antagonists (e.g., memantine) regulate glutamatergic activity to protect against excitotoxicity and are usually administered in moderate to severe cases.
● Medication may be administered to treat targeted neuropsychiatric symptoms: agitation, depression, or psychosis.
2. Cognitive and Behavioral Interventions
● Cognitive Stimulation Therapy (CST): Scheduled activities intended to promote memory, executive function, and social engagement.
● Reminiscence Therapy: Elicit discussions about previous life experiences in order to provoke thought and feelings.
● Reality Orientation Therapy: Orientations about time, place, and person can be helpful to combat confusion.
3. Lifestyle and Preventive Approaches
● Physical Activity: Engage in regular aerobic and resistance exercise, promoting neuroplasticity and vascular health.
● Dietary Interventions: A Mediterranean or DASH diet, rich in antioxidants and omega-3 fatty acids, may decrease neurodegeneration.
● Social Engagement: Interpersonal contact reduces cognitive decline and improves mood. 4. Caregiver Support and Environmental Interventions
● Established routines, environmental changes (e.g., reduce noise, provide clear signage), and assistive technologies can be helpful for the daily life of the patient.
● Caregiver education, stress management interventions, and respite care programs are necessary for long-term sustainable management.
A multidisciplinary approach combining pharmacological and behavioral strategies, in addition to caregiver support, continues to be the mainstay of dementia management. Early intervention is essential for optimal outcomes.
Preventive Strategies
While dementia has multiple risk factors, research suggests that lifestyle modifications and early interventions can significantly reduce the risk of cognitive decline.1. Cognitive Engagement
● Lifelong learning, reading, and problem-solving activities (e.g., puzzles, chess) help build cognitive reserve and delay the onset of dementia.
● Bilingualism and musical training have been linked to improved cognitive resilience. 2. Physical Activity
● Regular aerobic exercise (e.g., walking, swimming, cycling) improves cerebral blood flow and supports neuroplasticity.
● Strength training and balance exercises reduce fall risk and support overall brain health.
3. Heart-Brain Connection
● Managing hypertension, diabetes, and cholesterol through a healthy lifestyle and medications lowers the risk of vascular dementia.
● Smoking cessation and moderation of alcohol intake protect against neurodegeneration.
4. Nutrition and Diet
● A Mediterranean or DASH diet, rich in antioxidants, healthy fats, and whole grains, has been associated with a lower risk of dementia.
● Omega-3 fatty acids (found in fish, nuts, and seeds) and polyphenols (in berries, green tea, and dark chocolate) support brain function.
5. Social and Emotional Well-being
● Strong social connections reduce stress and cognitive decline. Engaging in community activities, volunteering, and maintaining relationships are key protective factors.
● Stress management techniques like mindfulness, meditation, and therapy help regulate cortisol levels, which impact brain health.
6. Sleep Hygiene
● Consistently getting 7–9 hours of quality sleep supports memory consolidation and reduces amyloid-beta accumulation, a hallmark of Alzheimer’s disease.
● Addressing sleep disorders, such as sleep apnea, is crucial for long-term brain health.
7. Avoiding Neurotoxic Exposure
● Limiting exposure to air pollution, heavy metals, and pesticides may lower dementia risk.
● Protective measures like wearing helmets and avoiding head trauma can prevent traumatic brain injury-related cognitive decline.
Early and sustained lifestyle interventions are key to reducing the risk of dementia. A proactive approach to brain health can help maintain cognitive function and overall well-being well into old age.